Benzodiazepines for Alcohol Withdrawal: The Gold Standard Treatment
Benzodiazepines for alcohol withdrawal remain the first-line medical treatment for safely managing moderate to severe withdrawal symptoms, preventing life-threatening complications like seizures and delirium tremens. These medications work by mimicking alcohol’s calming effect on the brain, restoring balance to the overexcited nervous system during the critical 48-72 hour window when most complications occur. Unlike over-the-counter remedies or self-tapering attempts, benzodiazepines follow evidence-based protocols that dramatically improve safety and completion rates.
For professionals seeking a structured home detox, understanding how benzodiazepines are used – dosing schedules, monitoring requirements, and safety criteria – is essential. This guide explains the clinical rationale, specific medications, protocols for home use, and how Liverehab’s Alcohol Recovery Home Detox programme incorporates prescription benzodiazepines with telehealth oversight to make safe withdrawal achievable without inpatient disruption.
For the complete withdrawal timeline where benzos are most critical, see our Alcohol Withdrawal Timeline guide.
Why Benzodiazepines Are Essential for Alcohol Detox
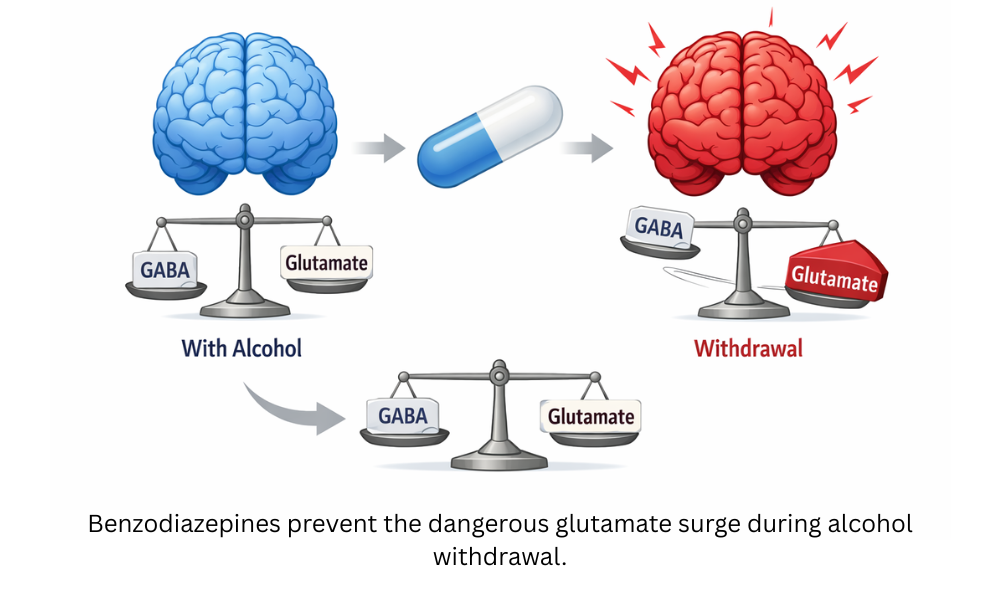
Chronic heavy alcohol use creates profound changes in brain chemistry. Alcohol artificially boosts inhibitory GABA activity while suppressing excitatory glutamate. When alcohol is suddenly removed, GABA levels crash while glutamate surges unchecked, creating dangerous brain hyperexcitability. This imbalance explains the tremors, anxiety, rapid heart rate, and insomnia of early withdrawal – and the seizures and delirium tremens that can follow in 2-5% of cases without treatment.
Benzodiazepines directly address this by binding to GABA receptors, safely restoring inhibition and preventing the “electrical storm” that causes complications. Clinical trials show benzodiazepines reduce seizure risk by 80% and delirium tremens incidence by similar margins when used according to protocol. The American Society of Addiction Medicine and NICE guidelines both name them the gold standard for moderate-severe withdrawal.
Without benzodiazepines – or with inadequate dosing – “cold turkey” attempts carry unacceptable risks, particularly for daily drinkers. Structured protocols using these medications turn a potentially dangerous process into a manageable medical event, whether in hospital or carefully supervised home settings.
Understand seizure risks in detail through our Critical Medical Risks guide in the complete Alcohol Detox & Recovery resource.
Which Benzodiazepines Are Used for Alcohol Withdrawal?
Different benzodiazepines are chosen based on their duration of action, liver metabolism, and the specific withdrawal protocol. Here’s the clinical breakdown:
| Medication | Duration | Best For | Typical Dosing Protocol |
| Diazepam (Valium) | Long | Symptom-triggered (CIWA-Ar) | 10-20mg every 1-4 hours as needed |
| Chlordiazepoxide (Librium) | Long | Fixed-schedule tapering | Loading dose 50-100mg, then taper |
| Lorazepam (Ativan) | Short | Liver impairment, elderly | 1-4mg every 4-6 hours |
| Oxazepam (Serax) | Short | Liver disease, minimal sedation | 15-30mg every 6-8 hours |
Diazepam remains most common due to smooth absorption and long half-life (20-50 hours), allowing steady coverage.
Lorazepam is preferred when liver function is compromised since it doesn’t require hepatic metabolism.
CIWA-Ar Protocol: The Clinical Institute Withdrawal Assessment for Alcohol scale scores symptoms (tremors, anxiety, agitation) from 0-67. Scores >8 trigger dosing; >15-20 indicate moderate-severe risk needing more aggressive intervention.
For full seizure prevention context, see our Alcohol Withdrawal Seizures guide.
How Benzo Protocols Work in Practice
Benzodiazepine protocols follow two main approaches, each with specific advantages depending on withdrawal severity and setting:
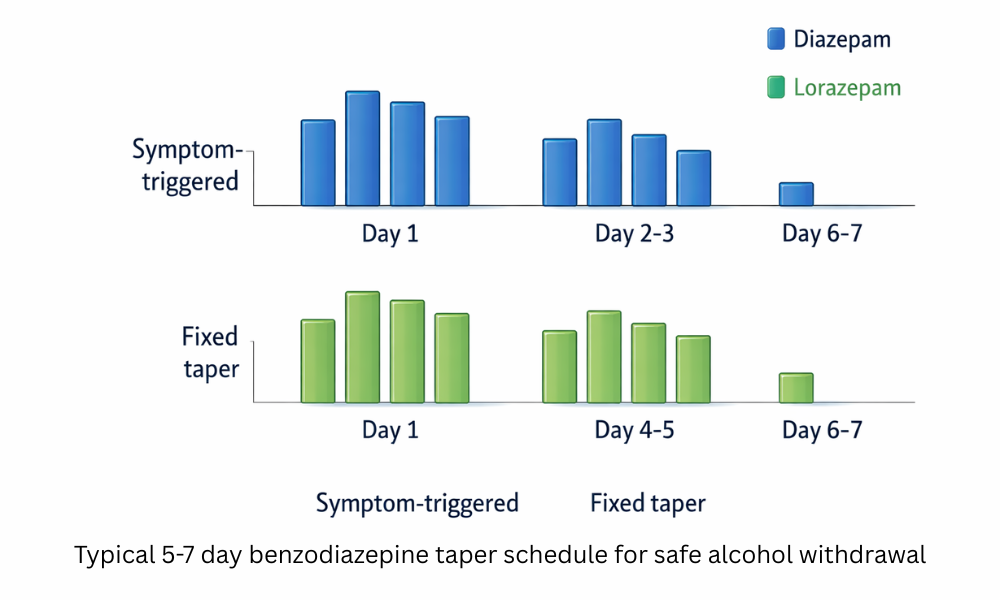
Symptom-Triggered Dosing (Preferred for Home Protocols): Uses the CIWA-Ar scale to dose only when symptoms reach threshold levels. Mild tremors or anxiety (score 8-15) trigger 10mg diazepam; moderate agitation or hallucinations (score 16-20) prompt 20mg; severe cases (>20) require loading doses and close monitoring. This minimizes total medication while preventing complications.
Fixed-Schedule Tapering (Hospital Standard): Begins with a loading dose (50-100mg chlordiazepoxide Day 1), then systematic reduction: 75% Day 2, 50% Day 3, 25% Day 4, complete by Day 5-7. Provides steady coverage for high-risk patients but risks oversedation in milder cases.
Home Protocol Adaptation: Lower starting doses (5-10mg diazepam equivalents) with twice-daily symptom logging. Clear escalation rules – if nausea prevents oral meds or confusion develops, immediate medical review required. Self-administration works because protocols match dose to predictable withdrawal curves, not guesswork.
Duration: Most complete taper by Day 5-7. Protracted use risks dependence, so protocols emphasize rapid but safe reduction.
Home Use of Benzodiazepines: Safe When Structured
Look, let’s be real – nobody wants to drive to a clinic every few hours for meds during detox. That’s why structured home protocols using benzodiazepines make so much sense for the right people. You get the same gold-standard medications doctors use in hospitals, but delivered in a way that fits your actual life.
Here’s how it works in practice: after a thorough screening confirms you’re low-to-moderate risk (no seizure history, stable vitals, no major medical red flags), you receive a precise prescription matched to your expected withdrawal curve. Maybe it’s diazepam 10mg every 6 hours days 1-2, tapering to 5mg days 3-4. You log symptoms morning and evening using a simple checklist, and if anything trends the wrong way, you follow the built-in escalation plan.
The beauty is in the predictability – Day 2 is always going to feel rougher than Day 4, so the protocol front-loads coverage when you need it most. You’re not guessing doses or hoping symptoms stay mild; you’re following the same CIWA-based system hospitals use, just from home. For professionals, this means you can handle emails or lighter calls while your body stabilizes, without anyone at work needing to know.
We’ve seen this work beautifully for executives, lawyers, surgeons – you name it. The key difference between “safe home benzo use” and “dangerous DIY” is the structure: clear criteria upfront, exact dosing schedule, symptom tracking, and zero ambiguity about when to call for help.
Risks & Side Effects to Understand
Even when used correctly under medical guidance, benzodiazepines come with risks professionals need to know before detox. The biggest concern is sedation – especially days 1-3 when doses peak. You might feel drowsy, have slower reflexes, or struggle with complex decision-making. This is why any responsible approach emphasizes getting immediate medical help if symptoms worsen.
Other side effects include mild confusion, unsteadiness, or next-day grogginess, particularly with longer-acting options like diazepam. Rebound anxiety can occur if tapering happens too fast, which is why established 5-7 day schedules are recommended rather than abrupt stops.
Tolerance is another reality – your body may adjust quickly, which is why fixed schedules prevent escalation. Respiratory depression is rare at withdrawal doses but explains why anyone with sleep apnea or lung issues should consult their doctor first.
The bottom line: Benzodiazepines are powerful tools, but they’re not DIY territory. If you’re considering them for detox, work with a healthcare provider who can assess your suitability and provide clear guidance. Always prioritize getting professional medical help if symptoms escalate beyond what’s expected – safety first.
Alternatives When Benzos Aren’t Suitable
Not everyone can or should use benzodiazepines for alcohol withdrawal. Liver impairment, respiratory issues, or previous adverse reactions make other options necessary. These alternatives provide effective symptom management while minimizing sedation risks.
Carbamazepine (Tegretol): Works by stabilizing neuronal membranes and reducing glutamate excitotoxicity. Studies show similar seizure prevention to diazepam with less cognitive impairment. Typical dose: 200mg twice daily, titrated to 400-600mg/day. Preferred for mild-moderate withdrawal.
Gabapentin (Neurontin): Modulates calcium channels to reduce excitatory neurotransmitter release. Effective for anxiety, insomnia, and cravings with minimal sedation. Starting dose: 300mg three times daily, up to 900-1800mg/day divided. Increasingly popular for home protocols.
Topiramate (Topamax): Dual action on GABA enhancement and glutamate inhibition. Reduces cravings while controlling seizures. Dose: 25mg daily, titrate to 100-200mg over 5-7 days.
Nutritional Support (Always Required): High-dose thiamine (100-500mg daily) prevents Wernicke encephalopathy. Magnesium 400mg nightly reduces tremors and hyperexcitability. Multivitamins address common deficiencies exacerbating symptoms.
These alternatives work best for milder withdrawal or as adjuncts. Anyone with moderate-severe risk should consult their doctor to determine the safest approach. Self-selecting medications without assessment carries unnecessary risks.
For vitamin protocols supporting withdrawal management, see our Vitamins & Nutrition for Alcohol Detox guide.
Getting Benzodiazepines Safely for Detox
Benzodiazepines are prescription-only medications that require professional medical evaluation before use. Live Rehab is not a medical detox solution nor do we recommend any specific treatment options. Here’s how to approach this responsibly.
Step 1: Consult Your Doctor
Schedule an appointment with your GP or addiction specialist. Be honest about your drinking pattern, duration, and any past withdrawal experiences. They will assess your risk level using clinical criteria and determine if benzodiazepines are appropriate.
Step 2: Understand the Prescription Process
Doctors typically prescribe based on severity:
- Mild withdrawal: May recommend monitoring or alternatives.
- Moderate risk: Short-term benzodiazepine course with taper instructions.
- High risk: Hospital referral or close outpatient follow-up.
Step 3: Never Self-Medicate
Using old prescriptions, buying online, or obtaining from friends is dangerous. Incorrect dosing risks oversedation, inadequate coverage, or rebound withdrawal. Always fill prescriptions through legitimate pharmacies.
Step 4: Pair With Structure
Even with a prescription, success depends on a clear plan. Log symptoms daily, follow exact dosing schedules, and have emergency contacts ready. Programs like Sobriety Success provide the non-medical framework—timing, nutrition, escalation rules—that complements medical treatment.
Important: If symptoms worsen (confusion, seizures, chest pain), seek emergency care immediately regardless of medication status.
How This Fits With a Home Detox Approach
Benzodiazepines fit perfectly into a structured home detox when used correctly under medical guidance. The key is combining a doctor’s prescription with a comprehensive non-medical framework that handles everything else.

Here’s how it works together:
Medical Component (Doctor Provides): Prescription, dosing instructions, and clinical assessment of your suitability.
Structural Component (Sobriety Success Provides): Daily symptom logging templates, precise timing schedules, nutrition protocols, hydration plans, and clear escalation rules for when to contact your doctor or seek emergency care.
Why This Combination Succeeds: Doctors give you the medication; the structured protocol gives you the method. You know exactly when to take each dose, what symptoms to expect at each stage, how to adjust your day around peak effects, and what constitutes a red flag requiring immediate medical attention.
For professionals, this means you can maintain lighter work responsibilities while detoxing safely at home, without the disruption of inpatient admission or the risks of going solo. The Sobriety Success method fills the gap between “here’s your prescription” and “here’s how to use it successfully at home.”
Liverehab’s Alcohol Recovery Home Detox programme delivers this exact integration: medical guidance coordination plus the complete Sobriety Success framework.
For the full picture on structuring detox around work demands, see our Can You Work During Alcohol Detox guide.
FAQ: Benzodiazepines for Alcohol Withdrawal
How long do you take benzodiazepines for alcohol withdrawal?
Typically 3-7 days following a taper schedule. Symptom-triggered protocols dose every 1-4 hours as needed days 1-3, then taper to complete by day 5-7. Fixed schedules load higher day 1 and reduce systematically.
Short-term therapeutic use (under medical guidance) carries low addiction risk. Protocols taper rapidly to prevent dependence. Misuse or abrupt cessation after detox creates rebound risks, which is why doctor supervision is essential.
Yes, for low-moderate risk individuals with a doctor’s prescription and structured protocol. Daily symptom logging and escalation rules prevent complications. High-risk cases (seizure history, liver disease) require closer medical oversight.
Discuss alternatives like carbamazepine or gabapentin. Nutritional support (thiamine, magnesium) remains essential. Any home detox must follow a clear safety framework regardless of medications used.
Ready to Detox Privately at Home?
No clinics. No explanations to colleagues. No disruption to your professional life.
Liverehab’s Alcohol Recovery Home Detox gives you the complete Sobriety Success framework—precise timing, symptom management, daily structure, and clear escalation rules—so you can detox safely in your own space while keeping work moving forward.
Privacy guaranteed. Home-based. Proven results.
Start Your Private Home Detox Now
Sources
- Alcohol Withdrawal Syndrome – StatPearls – NCBI Bookshelf
- Medications for Alcohol Use Disorder – AAFP
- Alcohol Withdrawal Symptoms & Treatment – American Addiction Centers
- Alcohol Withdrawal Timeline – The Recovery Village
- Alcohol Withdrawal Management – Cleveland Clinic
- Home Detox Safety Protocols – RehabsUK
Leave a Reply