What is Alcohol Detox & Why It Matters
Alcohol detoxification - often called detox - is the process your body undergoes when you stop drinking alcohol after prolonged, heavy use. It's not simply about removing toxins from your system; it's about allowing your body and brain to readjust to functioning without a substance they've become dependent on. When you've been drinking regularly, your body adapts to alcohol's presence. Your brain chemistry shifts, your central nervous system recalibrates, and over time, you develop both physical and psychological dependence. When alcohol is suddenly removed, withdrawal symptoms emerge as your system struggles to find its new baseline.
Detox is the critical first step in any addiction recovery journey, but it's often misunderstood. Many people believe detox alone is recovery it isn't. Detox is the foundation. It clears the acute physical dependence so your mind and body can be stable enough to address the deeper psychological, emotional, and behavioral factors that drive addiction. Without managing the physical withdrawal safely, most people relapse before they ever reach the therapeutic work that leads to lasting sobriety.
The stakes are significant. Alcohol use disorder (AUD) affects millions globally, and the consequences are severe. Alcohol-related deaths account for approximately 6% of global deaths each year, with over 3 million deaths attributed to excessive alcohol use worldwide (NCDAS). In many developed countries, alcohol-related mortality rates have increased by 40-65% over the past decade, reflecting both rising consumption and the dangers of untreated withdrawal. This isn't to alarm you - it's to underscore why getting this first step right matters.
Why detox must be medically managed. Alcohol withdrawal isn't like quitting other habits. It can be life-threatening. Withdrawal symptoms range from mild (tremors, anxiety, sweating) to severe (seizures, hallucinations, delirium tremens). Your heart rate can spike, blood pressure can fluctuate dangerously, and in the most severe cases, withdrawal can trigger seizures or delirium tremens - a condition with a mortality rate of 5-25% if left untreated. This is why attempting detox alone - often called "going cold turkey"—carries substantial risk. Medical supervision, appropriate medications, and professional monitoring can mean the difference between a safe recovery and a medical emergency.
The path forward. Whether you're considering detox for yourself or supporting someone else through this process, understanding what happens during withdrawal, knowing your treatment options, and recognizing when professional intervention is necessary are essential. This guide covers the complete picture: the medical realities of withdrawal, the treatment approaches available to you (inpatient, outpatient, and home-based detox), the medications that help manage symptoms, and how to choose the right path for your specific situation.
The good news: detox works. When done safely and with proper support, medical detoxification successfully breaks the acute physical cycle of dependence, preparing you for the psychological and behavioral work that leads to lasting recovery. Your body is remarkably resilient. With the right guidance, you can move through this challenging period and into a stable foundation for rebuilding your life.
Below, we explore everything you need to know about alcohol detox - from what happens in your body during withdrawal, to the medical risks you should understand, to the range of detox options available and how to decide which is right for you.
The Alcohol Withdrawal Timeline: What Happens in Your Body
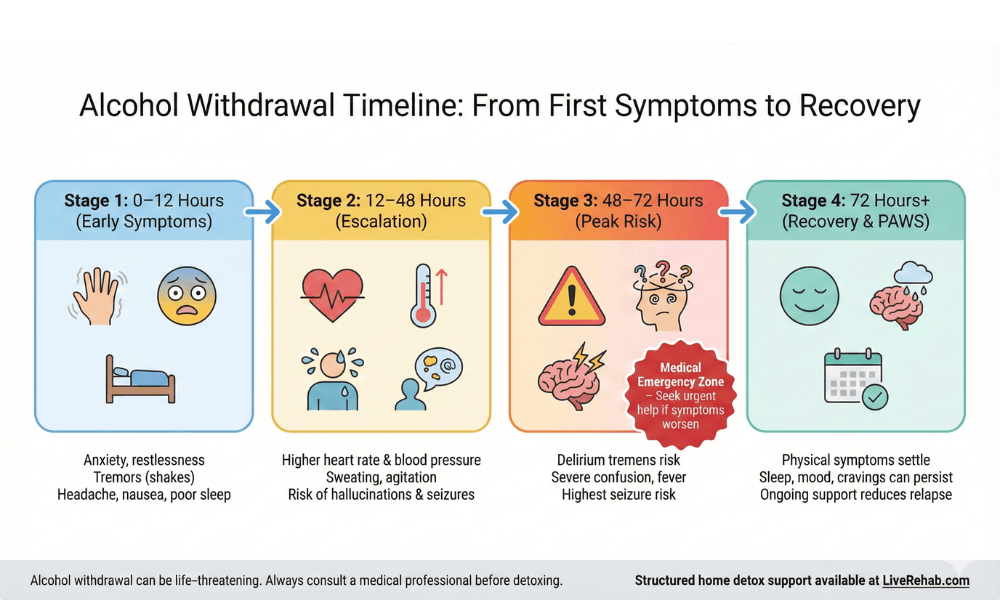
Alcohol withdrawal is a dynamic process that unfolds over several days, with symptoms that range from mild discomfort to life-threatening complications depending on the severity of physical dependence. Recognizing the stages and their key symptoms can help you gauge risk and know when medical intervention is crucial. Withdrawal typically begins 6–12 hours after the last drink and peaks around 48–72 hours, though some symptoms can linger for weeks or even months in certain cases.
Stage 1 (6–12 Hours): Early Symptoms
- Symptoms: Anxiety, headache, insomnia, shakes, nausea, and sweating commonly begin in this window as the nervous system becomes hyperactive in the absence of alcohol.
- Clinical Insight: For many, this period feels like a rough hangover, but it signals that physiological dependence has formed.
Stage 2 (12–48 Hours): Escalation & Hallucinations
- Symptoms: Confusion, elevated heart rate, increased blood pressure, and in some cases, hallucinations. Seizures can also begin in this window for heavy or long-term drinkers.
- Why It Matters: Symptoms reach their peak intensity during this period. Medical observation is recommended for anyone with a history of withdrawal complications.
Stage 3 (48–72 Hours): Severe Complications Risk
- Symptoms: Risk of delirium tremens (DTs)—marked by severe confusion, high fever, agitation, and possible seizures—peaks in this window. DTs occur in 5–15% of high-risk cases and are a medical emergency.
- Action Step: If symptoms worsen or seizures/hallucinations develop, emergency medical care is required.
Stage 4 (72 Hours+): Recovery or Protracted Symptoms
- Symptoms: Physical effects start to fade for most, but psychological symptoms (insomnia, anxiety, cravings) can persist for weeks. Known as Post-Acute Withdrawal Syndrome (PAWS), this stage requires ongoing emotional and medical support.
Critical Medical Risks: When Alcohol Withdrawal Becomes Dangerous
Alcohol withdrawal is not just uncomfortable; it can be medically life‑threatening in a subset of people, especially those with heavy long‑term use or prior complicated withdrawals. Serious complications like seizures, delirium tremens, and cardiovascular instability require immediate medical care and should never be managed with “cold turkey” at home. Understanding these risks helps you decide when a supervised detox (inpatient or structured home detox with medical oversight) is non‑negotiable.
Delirium Tremens (DTs): The Most Dangerous Complication
Delirium tremens is the most severe form of alcohol withdrawal and typically appears 48–72 hours after the last drink in high‑risk patients. It is characterized by profound confusion, agitation, disorientation, hallucinations, fever, and unstable vital signs, and is associated with a significant risk of death without prompt treatment.
DTs usually occur in people with a long history of heavy drinking, previous complicated withdrawals, or significant medical comorbidities. Because of the potential for rapid deterioration, anyone showing severe confusion, high fever, or dramatic behavior changes during withdrawal needs emergency medical evaluation.
Seizures During Alcohol Withdrawal
Withdrawal‑related seizures (usually generalized tonic‑clonic) often occur within 6–48 hours of the last drink and can happen even in people who otherwise look physically well. Having a history of previous withdrawal seizures, very high daily alcohol intake, or coexisting neurological conditions significantly raises this risk.
Seizures are more than a “scare”; they can lead to head injuries, aspiration, and progression to status epilepticus if not medically managed. This is one of the key reasons medical detox - whether inpatient or through a supervised home protocol with fast access to emergency care - is safer than trying to withdraw alone.
Cardiovascular & Autonomic Complications
As alcohol is removed, the autonomic nervous system becomes overactive, leading to spikes in heart rate and blood pressure. In people with underlying heart disease, uncontrolled hypertension, or advanced age, this surge can trigger arrhythmias, angina, or even heart attack or stroke.
Other autonomic complications include severe sweating, tremors, and temperature instability, all of which increase physical stress on the body. Continuous monitoring of vital signs and timely use of medication to control these parameters is a key part of safe detox protocols in both inpatient and well‑designed home‑based programs.
Wernicke–Korsakoff Syndrome & Nutritional Risks
Chronic heavy drinking often leads to severe deficiencies in thiamine (vitamin B1), which is essential for normal brain function. Acute thiamine deficiency can cause Wernicke encephalopathy—marked by confusion, loss of coordination, and eye movement abnormalities—and, if untreated, can progress to Korsakoff syndrome, a chronic, often irreversible memory disorder.
Because these conditions can be prevented or mitigated with timely thiamine and nutritional support, most evidence‑based detox protocols include vitamin supplementation before and during withdrawal. This is one of the clearest examples of why medically informed detox planning beats informal self‑detox attempts.
Who Is at Highest Risk of Complications?
Some people can safely withdraw with lower‑intensity support, but others face a significantly higher risk profile. High‑risk features include: past episodes of delirium tremens or withdrawal seizures, multiple prior detox attempts, very heavy daily alcohol intake, advanced age, serious heart or liver disease, and co‑occurring mental health conditions like severe depression or psychosis.
Anyone with these risk factors should be evaluated by a healthcare professional before attempting detox, even if they feel “fine” when they stop drinking. For this group, an inpatient setting or a tightly structured, medically overseen home detox protocol is not just safer - it can be lifesaving.
Learn how our home‑based detox protocol manages seizure risk safely
Your Detox Options: Inpatient, Outpatient, and Home Detox Explained
Choosing how to detox from alcohol is as important as choosing to detox at all. The right setting depends on your withdrawal risk, medical history, support system, and how much structure you need to stay safe and follow through. Below are the three main approaches people use to detox, with clear pros, cons, and who each option is best for.
Inpatient Medical Detox
Inpatient detox happens in a hospital or residential clinic where you live on-site for the first phase of withdrawal. You receive 24/7 monitoring, prescription medications, and immediate access to medical teams if complications arise. This setting is usually recommended for people with severe dependence, a history of seizures or delirium tremens, or other serious medical or mental health conditions.
The benefits include maximum safety, constant support, and complete removal from alcohol and triggers. The trade-offs are cost, time away from work and family, and less privacy. Many high-performing professionals find the disruption difficult but still need this level of care if their risk profile is high.
Outpatient Detox Programs
Outpatient detox allows you to live at home while attending scheduled appointments at a clinic or treatment center. You may receive medications, regular check-ins, therapy sessions, and monitoring of your vital signs, but you return home after each visit. This approach is generally suited to people with mild to moderate withdrawal risk who have a stable, supportive home environment.
Outpatient care offers more flexibility, lower cost, and less disruption to daily life than inpatient treatment. However, it also demands reliable transportation, strong personal discipline, and a home environment free from alcohol and major triggers. For some, the gaps between appointments can feel like a vulnerable window for cravings and relapse.
Supervised Home-Based Detox
Supervised home-based detox combines medical oversight and structured protocols with the privacy of staying in your own environment. Typically, it includes a thorough pre-assessment to confirm you are low to moderate risk, a clear medication and monitoring plan, and regular remote or telehealth check-ins during the critical withdrawal period. This is often the best match for high-functioning individuals who need to keep life as uninterrupted as possible while still prioritizing safety.
The advantages are discretion, the ability to keep working or caring for family, and a structured medical framework that is more robust than “going it alone.” You still need to meet suitability criteria, follow the plan closely, and have a clear escalation route if symptoms worsen. This is exactly where Liverehab’s alcohol home detox program fits: a structured, professional-grade pathway designed to support safe withdrawal at home for people who want privacy and real medical rigor, not guesswork.
Detox Options Overview
option | best for | monitoring level | key pros | key cons |
|---|---|---|---|---|
Inpatient | Severe dependence, high medical/psychiatric risk | 24/7 on-site care | Safest, full team support, no access to alcohol | Costly, disruptive, low privacy |
Outpatient | Mild–moderate withdrawal, strong home support | Scheduled clinic visits | Flexible, lower cost, live at home | Travel required, limited hours, more exposure to triggers |
Home-based | Lower–moderate risk, professionals needing privacy | Remote + structured check-ins | Discreet, work-compatible, structured plan | Requires suitability screening, strong self-discipline |
FDA-Approved Medications & Medical Protocols for Alcohol Detox
Medications are the cornerstone of safe alcohol withdrawal management, reducing symptom severity, preventing complications, and improving completion rates. No medication "cures" withdrawal, but evidence-based protocols use pharmaceuticals to stabilize the nervous system while your body readjusts. These are typically prescribed based on your risk profile and administered under medical supervision, whether inpatient, outpatient, or through a structured home detox program.
Benzodiazepines: The Gold Standard for Withdrawal
Benzodiazepines (e.g., chlordiazepoxide/Librium, diazepam/Valium, lorazepam/Ativan) are the first-line treatment for moderate-to-severe alcohol withdrawal. They enhance GABA activity—the brain's primary inhibitory neurotransmitter that's depleted during withdrawal—directly counteracting the dangerous hyperactivity that causes seizures and delirium tremens.
Dosing follows protocols like the CIWA-Ar scale (Clinical Institute Withdrawal Assessment for Alcohol), with symptoms tapered over 3–7 days to prevent rebound. While effective (reducing DTs risk by 80%), they require careful monitoring to avoid dependence or sedation in patients with liver impairment.
Naltrexone, Acamprosate & Disulfiram
These medications target post-detox relapse prevention rather than acute withdrawal:
- Naltrexone blocks opioid receptors, reducing alcohol's rewarding effects and cravings (50–60% relapse reduction in studies).
- Acamprosate restores glutamate-GABA balance disrupted by chronic drinking, helping maintain abstinence.
- Disulfiram causes unpleasant reactions if alcohol is consumed, serving as a strong deterrent.
Started after acute detox, these support long-term recovery when combined with therapy. They're particularly valuable in home-based protocols where ongoing adherence is key.
Vitamins & Nutritional Support
Chronic alcohol use depletes essential nutrients, amplifying withdrawal risks. Thiamine (Vitamin B1) is administered IV or orally first (100–500mg daily) to prevent Wernicke-Korsakoff syndrome—a potentially irreversible brain disorder causing confusion and memory loss.
Magnesium, multivitamins, folate, and electrolytes address deficiencies causing tremors, insomnia, and heart irregularities. Nutritional protocols in detox programs restore baseline function faster than supplements alone.
Gabapentin & Topiramate
For milder withdrawal or benzodiazepine intolerance:
- Gabapentin reduces cravings and anxiety by modulating glutamate; increasingly used off-label for alcohol detox.
- Topiramate stabilizes mood and seizures while curbing drinking urges via GABA enhancement and glutamate reduction[10].
These are adjuncts in structured programs, especially for patients needing to function at work during recovery[1].
Medical Monitoring During Detox
Vital signs (heart rate, blood pressure, temperature) are tracked every 4–8 hours during peak risk (24–72 hours). Blood tests assess electrolytes, liver function, and thiamine levels. Protocols include escalation criteria—if CIWA score >15 or seizures occur, benzodiazepine loading or hospitalization follows.
Remote monitoring via telehealth (with home pulse oximeters and daily video check-ins) makes this feasible in supervised home detox for low-moderate risk patients.
Factors That Affect Your Detox
What Determines Your Detox Timeline & Severity?
No two alcohol withdrawals are identical. The intensity, duration, and complications depend on individual biology, drinking history, and health status. Understanding these factors helps predict risks and choose the right detox approach—whether inpatient, outpatient, or supervised home-based. High-risk profiles demand professional oversight to avoid life-threatening issues.
Duration & Severity of Alcohol Use
Daily heavy drinkers (8+ units/day for men, 6+ for women) face more severe withdrawal than episodic binge drinkers. Long-term use (years vs. months) causes deeper neuroadaptations, prolonging symptoms up to 10 days vs. 3-5 days for lighter dependence. Quantity and pattern directly correlate with seizure/DTs risk.
Age & Overall Health
Older adults (over 65) experience worse outcomes due to slower metabolism, comorbidities, and reduced resilience—DTs risk doubles. Pre-existing conditions like liver cirrhosis, heart disease, or diabetes amplify cardiovascular strain during withdrawal's autonomic hyperactivity phase.
Co-occurring Mental Health Conditions
Anxiety, depression, or PTSD complicate 40-60% of AUD cases. These amplify psychological symptoms (insomnia, agitation) and relapse risk, often requiring dual-diagnosis protocols. Untreated mental health turns mild physical withdrawal into extended emotional turmoil.
Previous Withdrawal Episodes
"Kindling effect": Each detox attempt worsens the next due to brain sensitization. Prior seizures or DTs raise recurrence by 3-5x. Repeat withdrawers need escalated care, like benzodiazepine loading, to break the cycle safely.
Nutritional Status & Liver Health
Chronic alcohol depletes thiamine/magnesium, risking Wernicke encephalopathy. Elevated liver enzymes signal impaired drug metabolism, altering benzo dosing. Baseline nutrition tests guide supplementation - poor status extends recovery by days.
Recovery After Detox
What Comes After Detox: Long-Term Recovery Strategies
Detox clears the physical dependence but marks only the start of recovery. Without structured aftercare, relapse rates exceed 70% in the first year. Long-term success (50-60% sustained sobriety at 6-12 months) requires behavioral therapy, peer support, and relapse prevention to address the psychological roots of addiction.
The Role of Behavioral Therapy
Cognitive Behavioral Therapy (CBT) and motivational interviewing target triggers, coping skills, and thought patterns driving alcohol use. Studies show CBT reduces relapse by 40-50% when started post-detox. Sessions (weekly for 3-6 months) build resilience against cravings and high-risk situations.
Support Groups & Peer Communities
AA, SMART Recovery, or online groups provide accountability and shared experience. Regular attendance doubles long-term abstinence rates (up to 49% at 8 years vs. 25% without). For professionals valuing privacy, virtual meetings fit structured home recovery protocols seamlessly.
Medication-Assisted Treatment (MAT) for Long-Term Success
Post-detox, naltrexone (19% fewer heavy drinking days), acamprosate, or disulfiram extend sobriety. MAT combined with therapy yields 50-60% success at 6 months vs. therapy alone. Ideal for home-based continuity after acute withdrawal.
Aftercare Planning & Relapse Prevention
Personalized plans identify triggers (stress, social cues), set boundaries, and schedule check-ins. Relapse rates drop from 30% (year 1) to 7-10% (year 5+) with aftercare. Apps, coaching, and family involvement sustain momentum.
Addressing Underlying Mental Health
Dual diagnosis treatment for co-occurring anxiety/depression (40-60% of cases) integrates psychiatry with addiction care. Untreated mental health triples relapse risk; combined protocols boost 1-year sobriety to 60%+.
How to Choose the Right Detox Option for You
Decision Framework: Which Detox Approach Is Right for Your Situation?
Deciding on a detox path isn't one-size-fits-all—it's about matching your risk profile, lifestyle needs, and support resources to the safest, most effective option. Start with self-assessment: heavy daily drinking for years? History of seizures or DTs? Heart/liver issues? These red flags point to inpatient. Milder patterns with strong home stability lean toward outpatient or supervised home detox. The goal is zero guesswork: professional screening clarifies your category before symptoms hit.
Key questions to ask your doctor include your drinking quantity/pattern, prior withdrawal experiences, current medications, and mental health status. Bloodwork (liver enzymes, electrolytes) and a CIWA-Ar prediction score quantify risk objectively. For high-functioning professionals, privacy and work continuity often tip toward structured home protocols—if pre-screening confirms low-moderate risk and rapid escalation access. Inpatient suits undeniable medical complexity; outpatient fits those with reliable clinic proximity but home alcohol-free zones.
When Inpatient Detox Is Necessary: Severe cases—10+ years heavy use, past DTs/seizures, unstable vitals, or psychiatric crises—demand 24/7 oversight. Here, complication mortality drops near zero with IV meds and on-site teams. Cost and disruption are high, but so is the stakes; 5-15% untreated DTs risk justifies it.
When Outpatient Can Work: Mild symptoms, solid transportation, and sober home support make this viable. Daily check-ins manage benzos/thiamine, but gaps expose relapse windows. Success hinges on discipline; it's 20-30% cheaper than inpatient but fails without commitment.[12][15]
When Home-Based Detox Fits: Low-moderate risk (no prior seizures, <8 units/day, healthy vitals) plus telehealth monitoring and meds make privacy-compatible detox feasible for executives avoiding career hits. Protocols with daily vitals apps, video consults, and 24/7 escalation rival outpatient safety at home convenience - ideal when suitability is medically cleared first.
Never self-diagnose. A 5-minute specialist assessment reveals your fit, preventing "cold turkey" disasters. Liverehab's free screening matches you to the optimal path, often our professional home protocol for those balancing recovery with real life.
Frequently Asked Questions About Alcohol Detox & Recovery
How long does alcohol withdrawal last?
Alcohol withdrawal typically peaks at 48-72 hours and resolves physically within 5-7 days for most, though psychological symptoms like anxiety and cravings (PAWS) can persist 2-4 weeks or longer. Severity depends on drinking history—heavy chronic users may need 10+ days under supervision.
Can you detox from alcohol at home safely?
Yes, for low-moderate risk individuals (no prior seizures/DTs, <8 units/day, healthy vitals) with structured medical oversight, telehealth monitoring, and escalation plans. High-risk cases require inpatient care; self-detox risks seizures (5-15% incidence).
What are the first signs of alcohol withdrawal?
Symptoms start 6-12 hours post-last drink: anxiety, tremors ("shakes"), insomnia, nausea, sweating, and headache. These mild signs signal nervous system hyperactivity—monitor closely as escalation follows 12-48 hours later.
Is alcohol withdrawal dangerous without medical help?
Yes—untreated moderate-severe withdrawal carries 5-25% mortality from DTs, plus seizure and cardiovascular risks. Meds like benzodiazepines reduce complications by 80%; professional assessment is essential before starting.
What medications help with alcohol withdrawal?
Benzodiazepines (Valium, Librium) are first-line for symptoms/seizures; thiamine prevents brain damage. Post-detox, naltrexone/acamprosate curb relapse. Always under supervision—CIWA protocols guide dosing.
How long does it take to feel normal after detox?
Physical normalization: 7-10 days. Full cognitive/mood recovery: 1-3 months with aftercare. PAWS (fatigue, irritability) affects 10-25% up to 6 months; therapy/MAT accelerate this.
Can you drink alcohol while taking naltrexone?
Yes, technically—but naltrexone blocks euphoria, reducing reward and cravings (19% fewer heavy days). It's for maintenance post-detox, not during acute withdrawal. Combine with therapy for best results.
What is the difference between detox and rehab?
Detox (3-7 days) manages physical withdrawal medically. Rehab (28-90 days) addresses psychological/behavioral roots via therapy/support. 70% relapse without rehab; combined approaches yield 50-60% 1-year success.
Ready to Start Your Recovery? Next Steps
You've now seen the full picture: withdrawal unfolds predictably but dangerously without guidance, treatment options range from full inpatient to private home protocols, and lasting sobriety demands aftercare beyond detox alone. The common thread? Every successful path starts with professional assessment - matching your risk profile, lifestyle, and goals to the safest, most effective approach. Cold turkey fails 90%+ of the time; structured support transforms outcomes.
For high-performing individuals who refuse to let addiction derail career or privacy, Liverehab's Functional Recovery Protocol delivers medically rigorous home detox with telehealth monitoring, personalized meds, nutritional support, and seamless transition to ongoing coaching. No clinics, no stigma—just results in your own space.
Take action today: Explore Our Home Detox Program →
Why wait? 48 hours from now, symptoms could escalate. Secure your spot, get screened, and step confidently into recovery. Backed by clinical protocols, thousands of successes, and your commitment.
References
- Alcohol Withdrawal Syndrome - StatPearls - NCBI Bookshelf
- Alcohol Withdrawal Symptoms, Detox, Timeline, & Treatment - American Addiction Centers
- Alcohol Withdrawal Timeline - The Recovery Village
- Alcohol Withdrawal: Symptoms, Treatment & Timeline - Cleveland Clinic
- Alcohol Withdrawal Timeline & Symptoms – Priory Group
- Medications for Alcohol Use Disorder - AAFP
- Medications Development Program - NIAAA
- Pharmacotherapy for Alcohol Use Disorder - JAMA
- Alcohol Rehab Success Rates - Abbington House
- Does Rehab Work? Rehab Success Rates - WhichRehab
- Alcohol Relapse Rates & Statistics - The Recovery Village
- Alcoholics Anonymous Success Rates - American Addiction Centers
- Inpatient vs Outpatient Alcohol Detox - Rehab4Addiction
- Alcohol Detox at Home vs Rehab - RehabsUK
- Inpatient and Outpatient Treatment - NCBI
- The Alcohol Withdrawal Timeline - Atlanta Detox
- Alcohol Abuse Statistics 2025 - Drug Abuse Statistics
- Drug addiction: getting help - NHS