You can work during alcohol detox in some situations, but only if the detox is intentionally designed around safety, structure, and your professional life – never by “winging it” or trying to hide severe withdrawal from colleagues. The goal of this article is to show when it’s realistic to keep working, when it isn’t, and how a structured home detox (like Sobriety Success and the LiveRehab program) can make detox and work compatible for many high-performing people.
Can You Work During Alcohol Detox?
Many professionals delay getting help because they believe detox means disappearing into a clinic for weeks and risking their career. In reality, alcohol detox typically lasts 3 – 7 days and can often be done safely at home with a clear protocol, especially for people with low-to-moderate medical risk and a strong desire to maintain work continuity. The key is not whether you detox at home, but how you do it: following a structured plan, timing the process correctly, and being honest about your risk level.
A home-based detox using a step-by-step framework like Sobriety Success offers a realistic path: you stay in control of your schedule, you stay in your own environment, and you follow a designed process rather than hoping things don’t get out of hand. For many, that’s the only approach that feels compatible with a demanding job and real-world responsibilities.
What Alcohol Detox Actually Involves
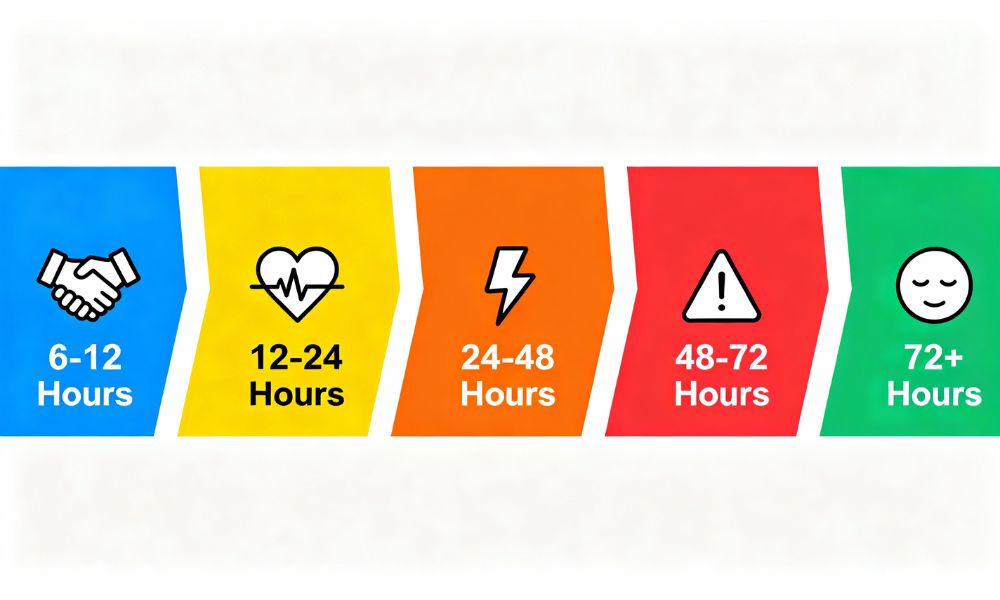
Alcohol detox is the process of letting your body clear alcohol and re-balance chemically after a period of regular or heavy drinking. This is when withdrawal symptoms appear – anything from mild anxiety and poor sleep to sweats, tremors, nausea, and, in a smaller subset of people, serious complications like seizures or delirium tremens. The most intense symptoms usually appear in the first 48–72 hours, then begin to ease, but the exact pattern depends on how heavily and how long you’ve been drinking.
Detox is not the entire recovery process; it’s the first stage. After detox, people still need to address cravings, habits, triggers, and emotional patterns. But in the detox window itself, the priority is safety and stability: managing symptoms, staying hydrated, eating properly, and having clear ground rules for what to do if things get worse instead of better. That’s why having a plan matters far more than the location.
For a complete hour-by-hour breakdown, see our Alcohol Withdrawal Timeline in the Alcohol Detox & Recovery Guide.
When It’s Not Safe to Work During Detox
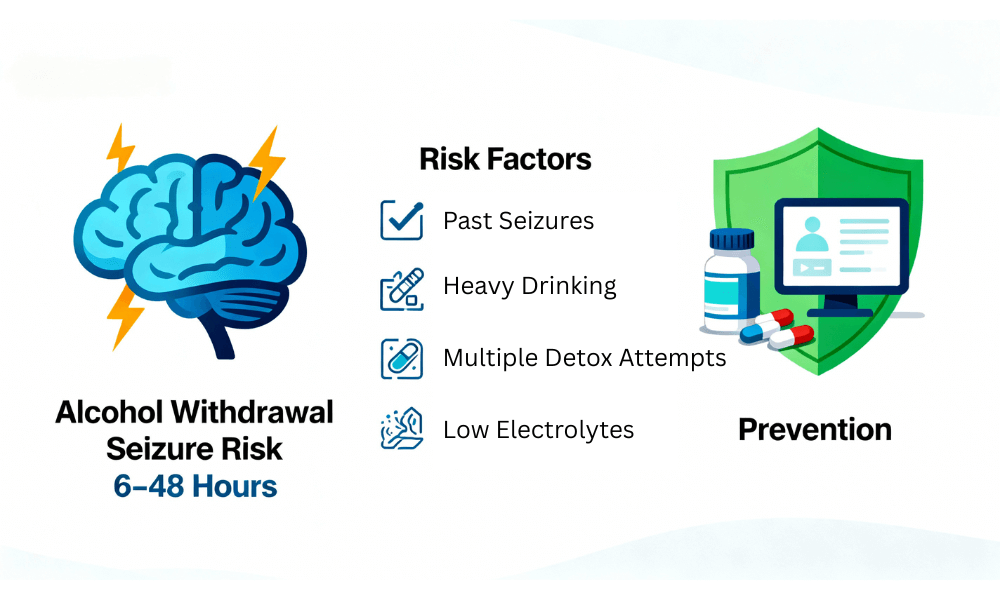
There are specific scenarios where trying to maintain work – especially office work, driving, or any safety-critical role – during detox is a bad idea. If you fit any of the following, you should treat detox as a medical event that requires you to step back from professional duties for a few days:
- History of withdrawal seizures, delirium tremens, or needing emergency care when you last stopped drinking.
- Very heavy, daily intake over many years (for example, drinking from morning into the evening most days).
- Significant heart, liver, or neurological problems that could be worsened by withdrawal stress.
- Serious mental health symptoms such as suicidal thoughts, severe anxiety attacks, or psychosis.
- No safe, stable home environment – chaotic living situation, no private space, or no one to contact if things deteriorate.
In these cases, the risk of complications is high enough that work should not be your priority during detox. You may still use a home-based protocol later in your journey – but the very first detox attempt should be approached with maximum safety. Pushing through emails, meetings, or driving to work while your body is in crisis is not courage; it’s unnecessary risk.
For full details on seizure/DTs risks, read the Critical Medical Risks section of our complete guide.
When You May Be Able to Work During Detox
On the other hand, many people fall into a low-to-moderate risk category where a structured home detox is absolutely realistic – and in some cases preferable – especially if they:
- Drink regularly and heavily, but not at the extreme end (for example, evenings only, with no prior seizures or hallucinations).
- Have no history of severe withdrawals, no major medical red flags, and are otherwise generally well.
- Have a reasonably calm, supportive home environment where they can rest between work blocks.
- Are willing to adjust their workload and expectations for a few days instead of pretending everything is “normal.”
For these people, the question isn’t “Can I work during detox?” but “How do I intelligently reduce and structure my work so detox and safety always come first?” A well-designed home protocol recognises that you may still answer emails, attend lower-stakes meetings, or continue remote work – but also that you’ll build in buffers, rest, and contingency plans so you’re not carrying the same load you normally would.
How a Structured Home Detox Can Fit Around Work

A structured home detox, like the approach laid out in Sobriety Success and Liverehab’s home programmes, is built for exactly this: making detox achievable without blowing up your career. The structure matters:
- Clear start date and planning: You don’t just “decide” to detox on a random Monday. You choose your start window, clear or reduce important commitments, and plan meals, hydration, and rest ahead of time.
- Staged days with expected symptom windows: You know which days are likely to be roughest (often days 2–3), and you plan those as your lowest-demand work days—more asynchronous work, fewer live calls.
- Built-in check-ins: You schedule times to log symptoms, gauge how you’re doing, and decide whether to ease back or continue.
- Boundary rules: You decide in advance what you won’t do on detox days—like driving long distances, making high-stakes presentations, or working late into the night.
Instead of trying to power through a full schedule, the home detox is designed around your work life: you maintain essential responsibilities while deliberately creating space for your body and brain to stabilise. That’s the difference between a serious home protocol and a DIY white-knuckle attempt.
Built for High-Performing Professionals
Liverehab’s Alcohol Recovery Home Detox is specifically designed for executives and professionals who need a structured, medically-supervised detox that fits around real work demands – not the other way around.
Practical Tips If You Plan to Work While Detoxing
If you’re a good candidate for home detox and are planning to work during it, treat this like a project that needs a realistic schedule, not wishful thinking. A few practical adjustments make a huge difference:
- Front-load and back-load important tasks. Shift high-impact work either before your detox start date or into the week after, so days 2–3 of detox are reserved for lighter tasks.
- Use remote work where possible. Working from home gives you control over your environment, reduces the stress of commuting, and allows you to take quick breaks as needed.
- Block your calendar. Put calendar holds for “focus blocks” and “recovery breaks” so people don’t book over them. Keep meetings shorter and spaced out.
- Tell one trusted person. You don’t need to disclose everything to everyone, but letting a trusted colleague or manager know you’re dealing with a health issue helps explain why you might be quieter or less available for a few days.
- Prioritise basics. Eat simple, nourishing food, drink plenty of water, and avoid extra caffeine and sugar that can spike anxiety and worsen sleep.

These are the details a structured approach should walk you through. A good protocol gives you “here’s what to expect on day X” and “here’s how to structure your day so detox and work don’t conflict.”
Do You Need Time Off After Detox?
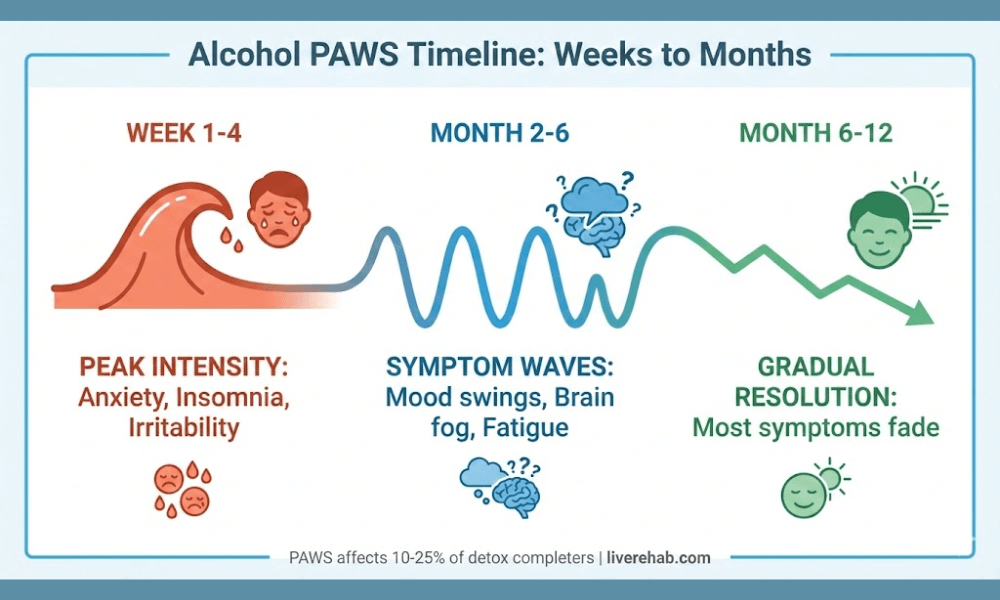
Even if you manage to work through all or most of your detox, it’s smart to assume you will not feel completely “normal” the moment acute symptoms pass. Many people experience what’s known as Post-Acute Withdrawal Syndrome (PAWS), which can include fatigue, poor focus, mood swings, and sleep issues for weeks or months after detox.
That doesn’t mean you can’t work; it means you should:
- Avoid scheduling the most critical projects or promotions immediately after detox.
- Give yourself a ramp-up period where you gradually take on more responsibility.
- Use routines, exercise, and ongoing support to stabilise your energy and mood.
How to Decide If Working During Detox Is Right for You
There isn’t a single answer that fits everyone. Instead, use this simple decision frame:
- If you’ve had severe withdrawals before, have serious medical conditions, or drink extremely heavily: Treat detox like a medical event. Work should pause, at least for the first few days, and you should seek direct medical input before attempting any home-based plan.
- If your pattern is heavy but not extreme, with no severe past withdrawals and you’re otherwise healthy: A structured home detox that explicitly accounts for your work schedule is often a safe and realistic option. You’ll still need to adjust your workload and follow a clear protocol, not improvise.
- If you’re somewhere in between: Get assessed. A brief conversation or assessment can help confirm whether you’re in the “safe at home with structure” category or whether more support is needed.
The real danger isn’t detoxing at home; it’s detoxing at home without a plan. A framework like Sobriety Success, combined with a tailored home detox programme, gives you the roadmap to balance safety, privacy, and professional life instead of choosing between your health and your career.
Find out if you’re a good fit for a structured home detox you can complete while working – learn more about our Alcohol Recovery Home Detox programme.
FAQ: Working During Alcohol Detox
Is it safe to go to the office during alcohol detox?
No. Office work, commuting, and driving are unsafe during detox due to seizure risk and impaired judgment. Remote work with a structured home protocol is safer for low-moderate risk individuals.
Absolutely not. Withdrawal impairs coordination, reaction time, and decision-making. Even mild symptoms make driving dangerous. Plan transportation or work remotely.
Most need to reduce workload for 3-5 days. Days 2-3 are typically peak symptoms. Structured home detox allows lighter remote work, but full intensity should wait until day 5+.
Stop immediately. Have a pre-planned emergency contact and medical escalation protocol. Never “tough it out” during detox – safety first.
Sources
- Alcohol Withdrawal Syndrome – StatPearls – NCBI Bookshelf
- Alcohol Withdrawal Symptoms, Detox Timeline – American Addiction Centers
- Alcohol Withdrawal Timeline – The Recovery Village
- Alcohol Withdrawal: Symptoms & Treatment – Cleveland Clinic
- Home Detox Safety Protocols – RehabsUK
- Medications for Alcohol Withdrawal – AAFP
- Relapse Prevention After Detox – Abbington House