We are excited to announce that ClearDay, our new sobriety and recovery support app, is now available on iOS. The Android version is already in progress and coming soon.
ClearDay was built for one clear purpose: to support people in recovery without adding noise, pressure, or unnecessary complexity. Whether you are addressing alcohol use, substances, compulsive behaviors, or any other pattern you are working to change, recovery often comes down to daily awareness, consistency, and self-honesty. ClearDay is designed to support exactly that.
Why We Built ClearDay
Many recovery apps try to do too much. They ask for accounts, email addresses, permissions, and ongoing engagement that can feel overwhelming, especially in early recovery. Others rely heavily on social features, streak pressure, or constant reminders that do not suit everyone.
ClearDay takes a different approach.
It is intentionally simple, private, and low friction. The app is designed to help you check in with yourself once a day, record how you are feeling, and then get out of your way. No feeds. No followers. No public profiles. No cloud sync by default.
Your data stays on your device.
A Recovery Tool That Respects Privacy
Privacy is not a feature add-on in ClearDay. It is the foundation.
ClearDay does not require you to create an account. There is no backend server storing your personal information. There is no analytics tracking your behavior. There are no ads. Everything you enter lives locally on your phone.
For many people in recovery, especially those navigating stigma, professional roles, family responsibilities, or simply wanting personal space, this matters. ClearDay is designed to feel safe to open, safe to use, and safe to keep.
What ClearDay Helps You Do
ClearDay focuses on the small, repeatable actions that actually support recovery over time.
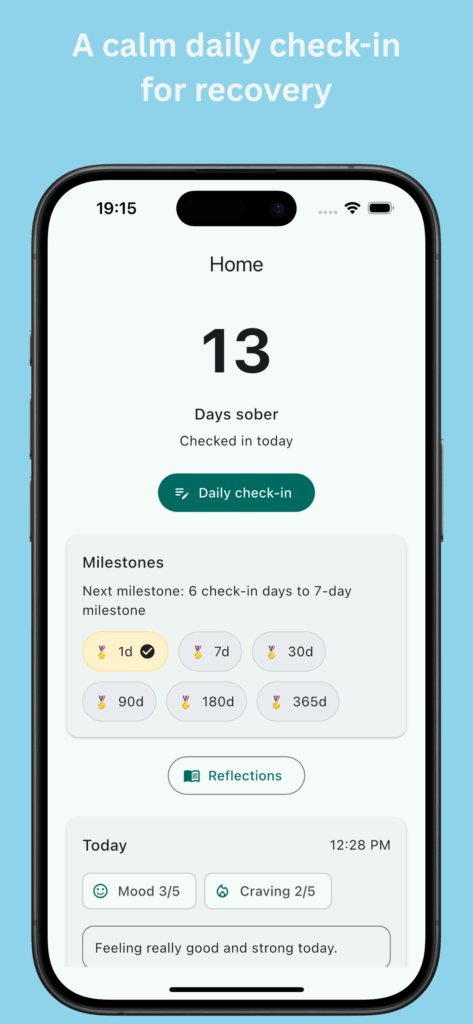
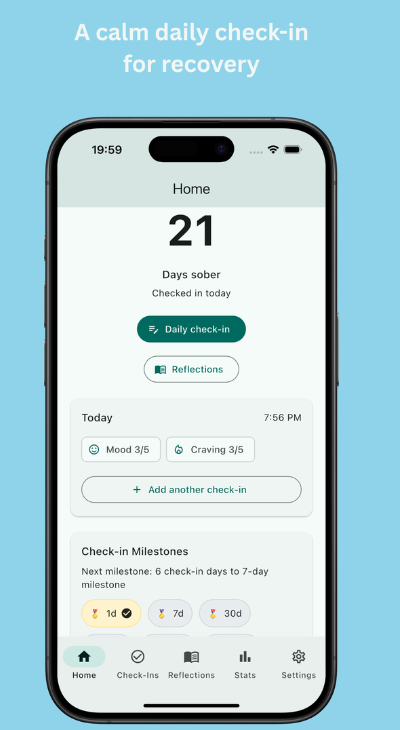
Each day, you can complete a quick check-in that takes less than a minute. You can rate your mood, note cravings, and optionally add a short reflection if something stands out. Over time, these check-ins create a clear picture of how you are doing, without requiring long journaling sessions or complex data entry.
The app also includes a sobriety tracker that shows your current streak and celebrates meaningful milestones. These moments are quiet and supportive, not flashy or competitive. They are there to reinforce progress, not create pressure.
You can also review past check-ins and reflections, helping you notice patterns such as how stress, sleep, routines, or specific situations affect your recovery. The goal is insight, not judgment.
Designed for Real Life, Not Perfect Days
Recovery does not happen in ideal conditions. It happens during busy mornings, stressful evenings, and moments when motivation is low.
ClearDay was designed with that reality in mind. The interface is calm and uncluttered. The flow is fast. You do not need to feel inspired to use it. You just need a few seconds of honesty.
Some days your check-in might be hopeful. Other days it might simply acknowledge that today is hard. Both are valid. ClearDay does not push toxic positivity or unrealistic expectations. It supports showing up as you are.
Click here to download it for free now: https://apps.apple.com/my/app/clearday-daily-reflection/id6757765724
Who ClearDay Is For
ClearDay is intentionally broad in who it supports. It is not tied to one recovery model, program, or philosophy.
It can be used alongside mutual aid groups, therapy, coaching, or medical support. It can also stand alone as a personal reflection tool if that feels right for you.
It is suitable for people in early recovery, people maintaining long-term change, and people who are still figuring out what recovery means for them. It is also useful for anyone who wants a private space to track urges, habits, and emotional patterns without labels.
Free to Use, With Thoughtful Expansion Planned
ClearDay is free to use with a complete core experience. Daily check-ins, reflections, milestone tracking, and basic stats are all available without payment.
In the future, optional paid features will be introduced for those who want deeper insights, such as advanced trend charts, guided reflection prompts, and voice reflections. These will always be optional, low-cost, and built with the same privacy-first principles.
There is no intention to turn ClearDay into a data-harvesting platform or a social network. Its role is simple support.
iOS Available Now, Android Coming Soon
ClearDay is now live on the Apple App Store for iPhone users. If you have been looking for a quiet, respectful tool to support your recovery, you can download it today.
The Android version is actively being developed and will be released soon. We wanted to launch on iOS first to ensure the experience is stable, polished, and aligned with our values before expanding.
A Final Word
Recovery is deeply personal. What works for one person may not work for another. ClearDay is not here to replace human connection, professional care, or community. It is here to support the small daily moments that often make the biggest difference.
If you value privacy, simplicity, and self-reflection, ClearDay was built for you.
We are proud to finally share it.
https://apps.apple.com/my/app/clearday-daily-reflection/id6757765724